Struggling to conceive can be a deeply emotional and frustrating experience for couples—and while much of the focus tends to fall on female fertility, male infertility is a factor in up to 50% of cases. The good news? Many causes of male infertility are treatable, especially with the help of a urologist who specializes in male reproductive health.
If you’re hoping to become a father and are facing challenges, a urologist might be one of your most important allies.
Understanding Male Fertility
Fertility in men largely depends on three key factors:
- Sperm production – Are you making enough healthy sperm?
- Sperm delivery – Is the sperm able to exit the body normally during ejaculation?
- Hormonal health – Are your testosterone and other hormone levels optimal?
When any of these systems is disrupted, fertility can be compromised. The causes can range from physical blockages to hormonal imbalances to lifestyle-related factors.
When to See a Urologist
Couples are generally advised to seek a fertility evaluation if they haven’t conceived after 12 months of regular, unprotected intercourse (or 6 months if the female partner is over 35). If there’s any history of testicular trauma, prior surgeries, infections, or low libido, the male partner should be evaluated sooner.
A male fertility urologist (sometimes called a reproductive urologist) is trained to assess and treat the full spectrum of male fertility issues, often in partnership with fertility specialists or reproductive endocrinologists.
What to Expect During a Male Fertility Workup
A male fertility evaluation begins with a detailed review of your medical, surgical, and sexual history. The urologist will also perform a physical exam focused on the testicles, penis, prostate, and signs of hormone imbalances (like decreased muscle mass or breast tissue).
Diagnostic tests may include:
- Semen analysis – Assesses sperm count, motility (movement), and morphology (shape)
- Hormone testing – Checks levels of testosterone, LH, FSH, and prolactin
- Scrotal ultrasound – Looks for conditions like varicoceles (enlarged veins in the scrotum)
- Genetic testing – May be recommended for men with extremely low or absent sperm counts
- Post-ejaculate urinalysis – To check for retrograde ejaculation
These tests help the urologist identify any treatable conditions and guide next steps in your fertility journey.
Common Causes of Male Infertility (and How Urologists Treat Them)
1. Varicocele
- What it is: Enlarged veins in the scrotum that increase temperature and impair sperm production.
- How it’s treated: Minimally invasive surgery (varicocelectomy) to repair the veins. This can significantly improve sperm quality and quantity.
2. Obstructive Azoospermia
- What it is: A condition where sperm is produced but blocked from exiting the body due to a prior vasectomy, infection, or congenital issue.
- How it’s treated: Microsurgical procedures to repair or bypass the blockage, or surgical sperm retrieval for use in assisted reproduction.
3. Non-Obstructive Azoospermia
- What it is: A condition where the testes are not producing enough (or any) sperm.
- How it’s treated: Treatment may include hormone therapy, lifestyle changes, or sperm retrieval techniques combined with IVF or ICSI (intracytoplasmic sperm injection).
4. Hormonal Imbalances
- What it is: Low testosterone or abnormal levels of LH/FSH can impact sperm production.
- How it’s treated: Medications like clomiphene citrate, hCG, or aromatase inhibitors to stimulate the body’s own testosterone and sperm production (without suppressing fertility, as testosterone replacement therapy often does).
5. Lifestyle Factors
- What it is: Obesity, smoking, excessive alcohol, drug use, or high heat exposure (e.g., hot tubs, laptops) can impair fertility.
- How it’s treated: Lifestyle modification, diet changes, and sometimes supplements like antioxidants to improve sperm quality.
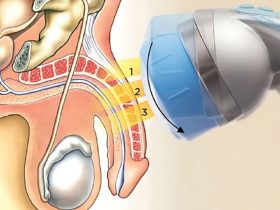
What About Sperm Retrieval?
In cases where sperm is not found in the semen but may still be present in the testicles, urologists can perform surgical sperm retrieval procedures, such as:
- TESA (Testicular Sperm Aspiration)
- TESE (Testicular Sperm Extraction)
- Micro-TESE (Microsurgical TESE) – More advanced and precise, used in cases of very low sperm production
These techniques allow men who previously believed they were sterile to become biological fathers using IVF and ICSI.
Working as a Team: Urologists and Fertility Clinics
Male fertility treatment is often part of a team-based approach. Urologists collaborate with fertility clinics to align treatment plans, optimize timing, and support the couple through assisted reproductive technologies if needed.
For some couples, treating a simple issue like a varicocele or low testosterone is enough to achieve natural pregnancy. Others may require sperm retrieval and IVF—but with modern tools, many pathways to parenthood are now possible.
Final Thoughts
Male infertility isn’t something to be ashamed of—and it’s not uncommon. If you and your partner are struggling to conceive, don’t assume the issue lies on one side. A complete fertility workup that includes a visit to a urologist can provide answers and open up new options.
You don’t have to navigate this journey alone. With expert evaluation and today’s advanced treatments, fatherhood may be closer than you think. We recommend urologist brooklyn.